
Biomarkers: small clues with a big impact
- Every patient is unique, and every case of lung cancer is unique
- Your doctor can learn more about your cancer by identifying clues inside your cancer cells, called biomarkers
- A biomarker can be a protein, gene or other substance in the blood or tumour tissue that can help guide treatment decisions
What can my biomarker tell me about my cancer?

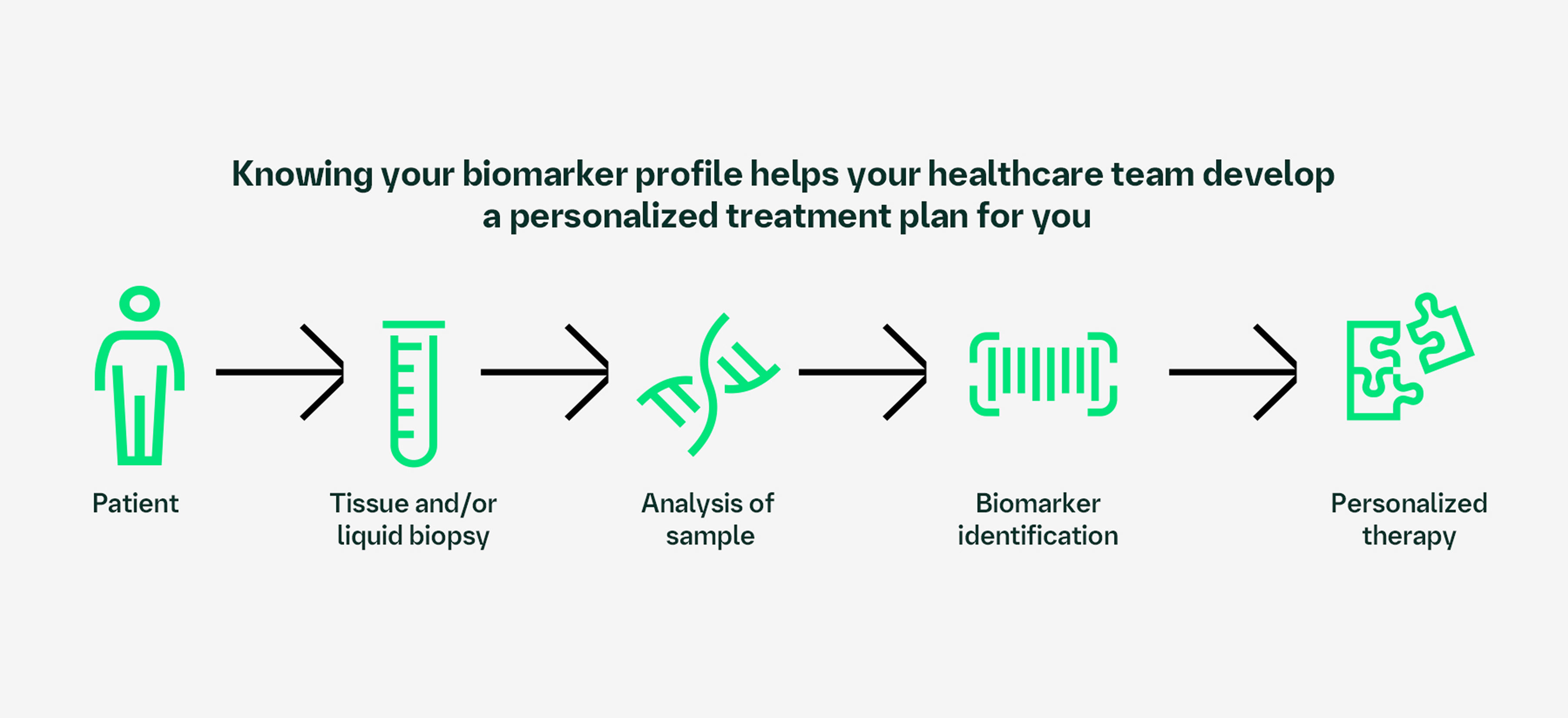
Some therapies target certain biomarkers. Testing for your cancer’s biomarker profile at diagnosis helps your healthcare team decide which treatment plan may work best for your unique lung cancer.
There are many different ways your doctor can test for biomarkers. What matters most is making sure a full panel of important biomarkers is checked–like HER2, EGFR, ALK and PD-L1–so your care team has the information needed to determine which targeted therapy may work best for you.
Identifying your biomarker profile
To learn about your biomarker profile, a sample of your tumour is collected and examined under a microscope. Your sample can be retrieved using a tissue or liquid biopsy.
You may feel nervous about your biopsy, but it is one of the most important steps in finding the best treatment option for you. Your healthcare team is there to answer any questions you may have about the procedure and to ensure you are safe and comfortable every step of the way.
Bronchoscopy: a thin, flexible tube is inserted through the mouth or nose into the lungs to collect a sample
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA): a thin, flexible tube is inserted through the mouth into the airways where a needle will collect a sample from the lymph nodes
- Transthoracic needle biopsy: a thin needle is inserted through the chest wall into the lung to collect a sample
What your biomarker means for your diagnosis
Your biomarker testing may include all or some of the following biomarkers:
HER2 (ERBB2) | MET | BRAF | KRAS | ROS1 |
EGFR | NTRK | ALK | RET | PD-L1 |
These biomarkers are often found in healthy cells and act as a light switch to help regulate cell growth and division. Normally, cells cycle between “on” and “off”, growing when needed and resting when not. In cancer, changes to the tumour’s DNA can cause these biomarkers to get stuck in the “on” position, breaking the cycle and making your cells grow too quickly.
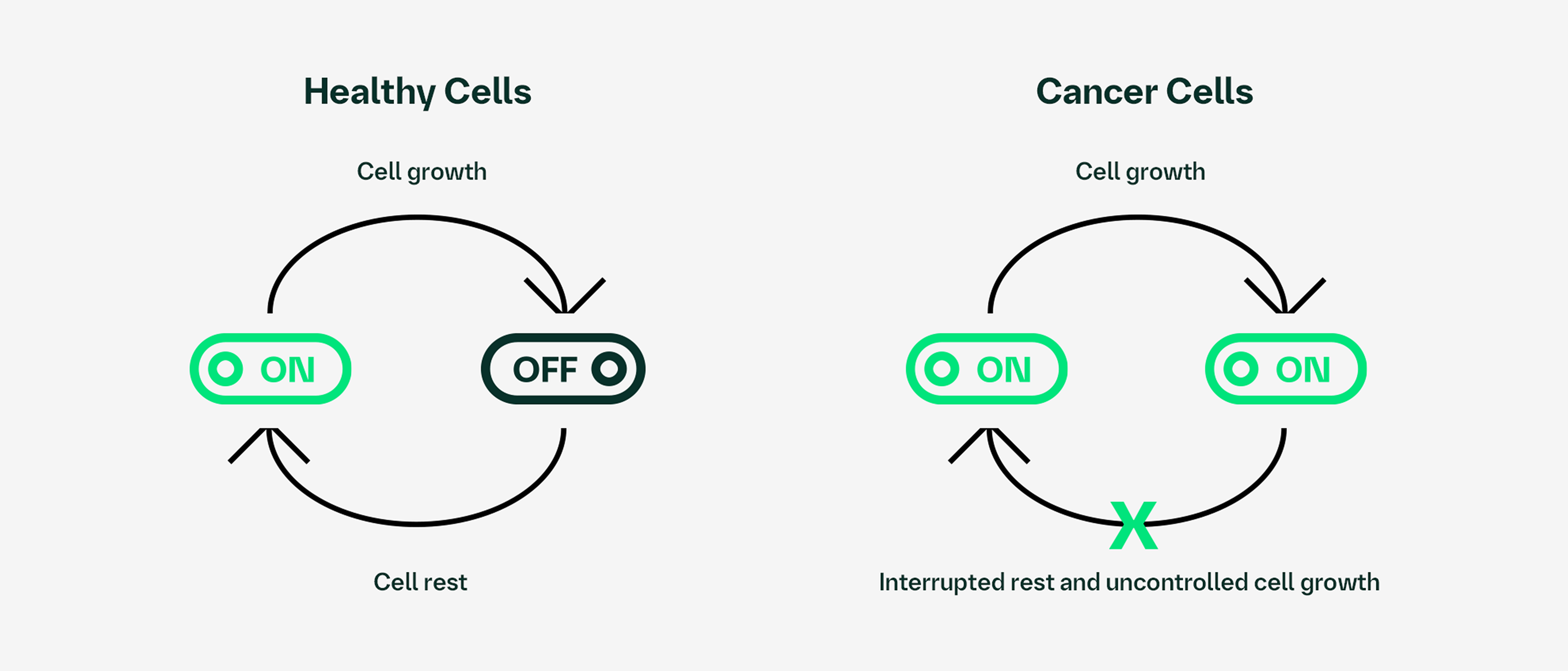
Your biopsy results can show which biomarker is driving cell growth in your tumour. From here, your doctor can identify available treatment options that target your biomarker.
HER2=human epidermal growth factor receptor 2; EGFR=epidermal growth factor receptor; ALK=anaplastic lymphoma kinase; PD-L1=programmed death-ligand 1; ERBB2=erb-B2 receptor tyrosine kinase 2; MET=mesenchymal epithelial transition factor receptor; BRAF=v-raf murine sarcoma viral oncogene homolog B; KRAS=Kirsten rat sarcoma viral oncogene homolog; ROS1=c-ros proto-oncogene 1; NTRK=neurotrophic tyrosine receptor kinase; RET=rearranged during transfection.


